- Diabetes Foot
- Varicose Veins
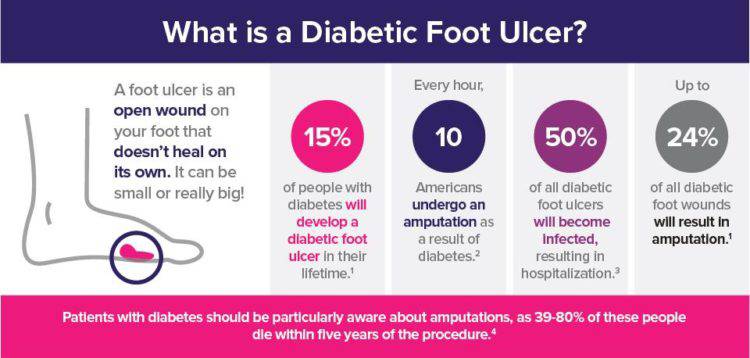
What Is a Diabetic Foot Ulcer?
A diabetic foot ulcer is an open sore or wound that occurs in approximately 15 percent of patients with diabetes, and is commonly located on the bottom of the foot. Of those who develop a foot ulcer, six percent will be hospitalized due to infection or other ulcer-related complication. Diabetes is the leading cause of nontraumatic lower extremity amputations, and approximately 14 to 24 percent of patients with diabetes who develop a foot ulcer have an amputation. Research, however, has shown that the development of a foot ulcer is preventable.
Who Can Get a Diabetic Foot Ulcer?
Anyone who has diabetes can develop a foot ulcer. Native Americans, African Americans, Hispanics and older men are more likely to develop ulcers. People who use insulin are at a higher risk of developing a foot ulcer, as are patients with diabetes-related kidney, eye, and heart disease. Being overweight and using alcohol and tobacco also play a role in the development of foot ulcers.
What Is the Value of Treating a Diabetic Foot Ulcer?
Once an ulcer is noticed, seek podiatric medical care immediately. Foot ulcers in patients with diabetes should be treated for several reasons:
- To reduce the risk of infection and amputation
- To improve function and quality of life
- To reduce health care costs
How Should a Diabetic Foot Ulcer Be Treated?
The primary goal in the treatment of foot ulcers is to obtain healing as soon as possible. The faster the healing of the wound, the less chance for an infection.
- Prevention of infection
- Taking the pressure off the area, called “off-loading”
- Removing dead skin and tissue, called “debridement”
- Applying medication or dressings to the ulcer
- Managing blood glucose and other health problems
Not all ulcers are infected; however, if your podiatric physician diagnoses an infection, a treatment program of antibiotics, wound care, and possibly hospitalization will be necessary.
Preventing Infection
There are several important factors to keep an ulcer from becoming infected:
- Keep blood glucose levels under tight control/li>
- Keep the ulcer clean and bandaged/li>
- Cleanse the wound daily, using a wound dressing or bandage/li>
- Do not walk barefoot
Off-Loading
For optimum healing, ulcers, especially those on the bottom of the foot, must be “off-loaded.” Patients may be asked to wear special footgear, or a brace, specialized castings, or use a wheelchair or crutches. These devices will reduce the pressure and irritation to the ulcer area and help to speed the healing process.
The science of wound care has advanced significantly over the past ten years. The old thought of “let the air get at it” is now known to be harmful to healing. We know that wounds and ulcers heal faster, with a lower risk of infection, if they are kept covered and moist. The use of full-strength betadine, peroxide, whirlpools and soaking are not recommended, as this could lead to further complications.
Applying Medication and Dressings
Appropriate wound management includes the use of dressings and topically-applied medications. These range from normal saline to advanced products, such as growth factors, ulcer dressings, and skin substitutes that have been shown to be highly effective in healing foot ulcers.
For a wound to heal there must be adequate circulation to the ulcerated area. Your podiatrist may order evaluation test such as noninvasive studies and or consult a vascular surgeon.
Managing Blood Glucose
Tightly controlling blood glucose is of the utmost importance during the treatment of a diabetic foot ulcer. Working closely with a medical doctor or endocrinologist to accomplish this will enhance healing and reduce the risk of complications.
Surgical Options
A majority of noninfected foot ulcers are treated without surgery; however, when this fails, surgical management may be appropriate. Examples of surgical care to remove pressure on the affected area include shaving or excision of bone(s) and the correction of various deformities, such as hammertoes, bunions, or bony “bumps.”
Healing Factors
Healing time depends on a variety of factors, such as wound size and location, pressure on the wound from walking or standing, swelling, circulation, blood glucose levels, wound care, and what is being applied to the wound. Healing may occur within weeks or require several months.
How Can a Foot Ulcer Be Prevented?
The best way to treat a diabetic foot ulcer is to prevent its development in the first place. Recommended guidelines include seeing a podiatrist on a regular basis. He or she can determine if you are at high risk for developing a foot ulcer and implement strategies for prevention.
You are at high risk if you:
- Have neuropathy
- Have poor circulation
- Have a foot deformity (i.e. bunion, hammer toe)
- Wear inappropriate shoes
- Have uncontrolled blood sugar
Reducing additional risk factors, such as smoking, drinking alcohol, high cholesterol, and elevated blood glucose are important in the prevention and treatment of a diabetic foot ulcer. Wearing the appropriate shoes and socks will go a long way in reducing risks. Your podiatric physician can provide guidance in selecting the proper shoes.
Learning how to check your feet is crucial in noticing a potential problem as early as possible. Inspect your feet every day—especially between the toes and the sole—for cuts, bruises, cracks, blisters, redness, ulcers, and any sign of abnormality. Each time you visit a health care provider, remove your shoes and socks so your feet can be examined. Any problems that are discovered should be reported to your podiatrist or a medical professional as soon as possible, no matter how “simple” it may seem to you.
The key to successful wound healing is regular podiatric medical care to ensure the following “gold standard” of care:
- Lowering blood sugar
- Appropriate debridement of wounds
- Treating any infection
- Reducing friction and pressure
- Restoring adequate blood flow
What are Varicose Veins and spider veins?
Varicose Veins are dilated, elongated and tortuous veins Varicose (VAR-i-kos) veins are enlarged veins that can be blue, red, or flesh-colored. They often look like cords and appear twisted and bulging. They can be swollen and raised above the surface of the skin. Varicose Veins are often found on the thighs, backs of the calves, or the inside of the leg. During pregnancy, Varicose Veins can form around the vagina and buttocks. Spider veins are like Varicose Veins but smaller. They also are closer to the surface of the skin than Varicose Veins. Often, they are red or blue. They can look like tree branches or spider webs with their short, jagged lines. They can be found on the legs and face and can cover either a very small or very large area of skin. It is classified by ICD10 as I 183 diseases

What causes Varicose Veins and spider veins?
Varicose Veins can be caused by weak or damaged valves in the veins. The heart pumps blood filled with oxygen and nutrients to the whole body through the arteries. Veins then carry the blood from the body back to the heart. As your leg muscles squeeze, they push blood back to the heart from your lower body against the flow of gravity. Veins have valves that act as one-way faps to prevent blood from flowing backward as it moves up your legs. If the valves become weak, blood can leak back into the veins and collect there. (This problem is called venous insufficiency.) When backed-up blood makes the veins bigger, they can become Varicose Veins.
How common are abnormal leg veins?
About 50 to 55 percent of women and 40 to 45 percent of men in the United States suffer from some type of vein problem. Varicose Veins affect half of the people 50 years and older. In India, the exact research is not carried out and the percentage is less common than the US still it is quite common.
What factors increase my risk of Varicose Veins and spider veins?
Many factors increase a person’s chances of developing varicose or spider veins. These include:
- Increasing age: As you get older, the valves in your veins may weaken. S
- ex females: More prone to Varicose Veins.
- Weight: Persons who are obese have more chances of Varicose Veins.
- Heredity: Genes play a major role in developing Varicose Veins.
- Hormonal changes: These occur during puberty, pregnancy, and menopause. Taking birth control pills and other medicines containing estrogen and progesterone also may contribute to the forming of varicose or spider veins.
- Pregnancy: During pregnancy, there is a huge increase in the amount of blood in the body. This can cause veins to enlarge. The growing uterus also puts pressure on the veins. Varicose Veins usually improve within 3 months after delivery. More Varicose Veins and spider veins usually appear with each additional pregnancy.
- Lack of movement: Sitting or standing for a long time may force your veins to work harder to pump blood to your heart. This may be a bigger problem if you sit with your legs bent or crossed.
- Sun exposure: This can cause spider veins on the cheeks or nose of a fair-skinned person. Most varicose and spider veins appear in the legs due to the pressure of body weight, force of gravity, and task of carrying blood from the bottom of the body up to the heart. Compared with other veins in the body, leg veins have the toughest job of carrying blood back to the heart. They endure the most pressure. This pressure can be stronger than the one-way valves in the veins.
How will I be diagnosed?
You will be diagnosed on a physical exam. The doctor will look at your legs while you are standing or sitting and ask about your symptoms/pain. The doctor will then do a venous duplex ultrasound, which is used to see the veins’ structure, check the blood flow in your veins, and look for blood clots. This test uses sound waves to create pictures of structures in your body.
What are types of Varicose Vein?
They are of 3 types:
- Trunk Varicose Vein
- Reticular Varicose Vein are red
- Telangiectasiae or spider or thread veins
What is venous reflux?
Normally, veins in the lower extremities carry blood to the heart against gravity. This is accomplished by one-way valves, which allow blood to flow upwards while your muscles contract. When your muscles relax, the valves snap shut preventing blood to flow in the wrong direction (towards your feet).
When veins become weak and the valves in your veins become faulty, blood is allowed to flow in the wrong direction (towards your feet). This puts excess pressure on the vein walls, which causes them to expand further. This expansion causes the valves to be even more ineffective.
The most common veins to reflux are called saphenous veins. Visible varicose and spider veins are typically branches coming from these veins.
What is venous insufficiency?
Venous insufficiency is the medical condition in which the valves in the lower extremities do not function properly, causing a variety of symptoms (varicose and spider veins). Venous insufficiency is synonymous with venous reflux.
When should I consult a doctor?
With safe, effective treatments readily available, you no longer need to suffer from varicose or spider veins. If you think you have a problem, you should consult a vein specialist. Even without the presence of Varicose Veins, if you suffer from aching leg pain, fatigue/heaviness of the legs, or swelling and pruritus (itchy legs), you may be suffering from venous insufficiency. These symptoms usually get worse as the day progresses, and you may get some relief by elevating your legs. Other symptoms include restless legs, night cramps, and, in severe cases, skin color changes and bleeding skin ulcers.
How long does recovery take?
Immediately after Varicose Vein treatment, you will be able to resume most normal activities; exceptions are heavy lifting, extreme exercise, and application of heat to the treated extremity. Usuall,y you can resume heavy exercise in approximately two weeks. Complete recovery times vary from person to person. For spider vein treatment there is no significant recovery time and patients experience minimal if any bruising.
Is venous insufficiency related to restless leg syndrome?
Restless Leg Syndrome is a medical condition associated with the constant desire to move the limbs because of perceived unpleasant sensations in them. The symptoms can include itchiness, pain, throbbing, aching, fidgets, tearing, and a ‘creepy crawly’ sensation.From the vein world end, venous insufficiency is one cause (not the only cause) of restless legs and there is evidence that treating venous insufficiency can benefit some patients who suffer from restless legs.
Do men get Varicose Veins?
Yes. Women, however, experience more vein problems than men mainly because of the unique additional risk factors for females, including estrogen levels and pregnancy.
Is it safe during pregnancy?
We recommend avoiding vein treatments while pregnant or if you are breastfeeding since the procedures are elective and medications may be necessary. Additionally, we recommend waiting several months after pregnancy for treatment, since Varicose Veins may improve or resolve in that time.
What is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis refers to the formation of a blood clot (thrombus) in the deep veins of the body, most commonly the lower extremities. A thrombus may form as a result of a blood-clotting abnormality, an injury, or a period of prolonged inactivity (such as a long airplane ride or bed rest). One of the dangers of a DVT is that a thrombus can break loose and travel through the bloodstream to the lungs, resulting in a life-threatening pulmonary embolism. Another danger of DVT is known as a post-thrombotic syndrome. This occurs when the valves of the deep venous system are damaged, resulting in long-term symptoms including pain, swelling, and discoloration of the skin.
A person with deep vein thrombosis may or may not have symptoms. Symptoms include tenderness, pain, or swelling. Treatment usually includes the use of blood-thinning medications (anticoagulants) that prevent new clots from forming or prevent existing clots from getting larger. Newer catheter-directed therapies are available, including devices that remove clots, administer drugs directly into a clot, or both. Procedures of this kind typically are done by an interventional radiologist.
What is Economy Class Syndrome?
Economy Class Syndrome refers to the occurrence of deep vein thrombosis (blood clots in the deep veins of the legs) in air travelers, placing them at risk for pulmonary embolism (blood clot traveling to the lungs). The pulmonary embolus can cause sudden death. It is thought that the cause of venous thrombosis in air travelers is related to immobilization and dehydration. There are multiple underlying medical conditions that place some individuals at even higher risk. In order to avoid the economy class syndrome, it is prudent to maintain adequate hydration, move around the cabin as much as possible and perform calf muscle exercises. Additionally, there is medical evidence to suggest that wearing medical compression stockings reduces the risk of blood clots. If you are at high risk of forming blood clots, your physician may prescribe aspirin or low molecular weight heparin.
Are all lasers equal?
All lasers are not created equal. While all of the lasers on the market attempt to damage the targeted vein wall in order to close it shut, the methods by which they do so differ. The first generation of lasers targeted the blood within veins, which resulted in excessive heat. Though the heated blood would eventually damage the vein wall as intended, the excessive heat caused tiny holes in the vein which then leaked blood and caused bruising. Newer laser systems such as Biolitec’sELVeS PL-1470nm Laser System Thermalite 1470 directly target the water within the vein wall, causing it to shut close. Because these laser systems can do this with far less heat, there is much less bruising.
Can Varicose Veins reoccur?
Yes, most commonly recurrences are due to the formation of new veins or from untreated sources of venous reflux, it is a chronic progressive disease.
Who is a Phlebologist?
A Phlebologist is a physician who specializes in the treatment of veins. Does removal of these veins affect coronary artery bypass surgery later? No, these diseased veins cannot be used as conduits for bypass surgery as the lumens are not healthy. Otherwise, also conduits now used are mainly arterial and thus will not be affected by the absence of superficial veins of the legs.

